When accessing C-19 risk factors, some are obvious like obesity. Others aren’t so conspicuous like low calcitriol or high blood sugar. So you can’t always look at a so-called “perfectly healthy” person, especially without seeing that person’s blood work, and assume that such a person actually is “perfectly” healthy. More often than not, such a person is NOT “perfectly” healthy.
So do you know if you’re selective IgA deficient or SIgAD?
It’s a very common immune deficiency that may or may not present autoimmune symptoms. Per the top paper below, SIgAD occurs in every 1 out of 120 Caucasians. Another source from the Cleveland Clinic put that figure at 1 out of 500 Caucasians. Either way, that’s still a high figure. The numbers are lower in different racial groups including Asians.
What is SIgAD?
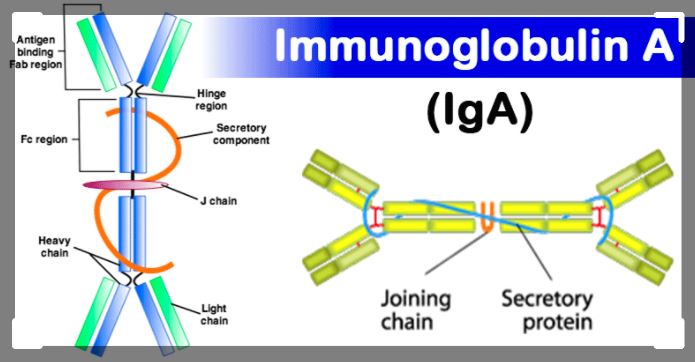
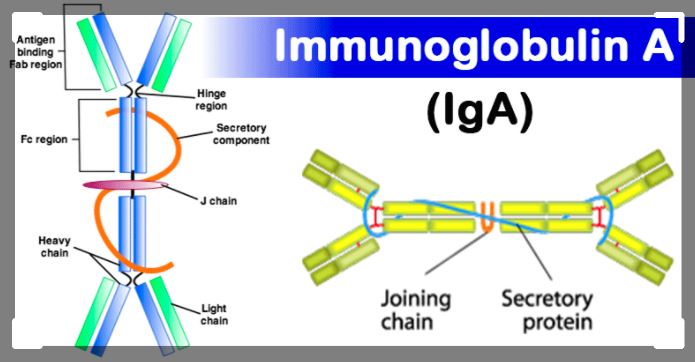
It’s having low levels of IgA antibodies while having normal levels of IgM and IgG antibodies. Here’s another definition from the paper from Italy below: “Selective IgA Deficiency (SIgAD) is a primary immunodeficiency characterized by an undetectable level of immunoglobulin A in the blood and secretions but no other immunoglobulin deficiencies.”
There are basically three types of IgA antibodies: IgA, IgA1 and IgA2 antibodies. IgA1 and IgA2 antibodies are in your secretive fluids and mucosal linings of your respiratory and digestive tracts. So if you’re deficient in IgA antibodies, you have less immunity against pathogens that enter your nose and mouth especially respiratory mucosal viruses like influenza and Sars-C0V-2
Here is a really interesting paper (accepted manuscript) from the Japanese Journal of Infectious Diseases on this topic: Relationship between selective IgA deficiency and C0VlD-19 prognosis
Another published paper from Italy also on this topic:
IgA Antibodies and IgA Deficiency in SARS-CoV-2 Infection
Both of these papers find a strong correlation between people who have selective IgA deficiency [SIgAD] and people who are much more prone to adverse outcomes if infected with Sars-C0V-2. The paper in the Japanese Journal notes that there’s a 7.7 fold increase of likelihood of severe C-19 if a person is SIgAD.
- The paper details the possible mechanistic reasons for this poorer prognosis for SIgAD patients with C0VlD-19 as follows:The low IgA level does not adequately neutralize infectious viruses approaching the mucosal immune barrier
- More SARS-C0-2 particles than normal cross the mucosa
- The increased antigen (viral) load sensitizes T and B cells, and thus increases the risk of autoimmunity, cytokine storm syndrome and acute respiratory distress syndrome [ARDS]. The incidence of autoimmune diseases is higher in SIgAD patients. In such patients, the risk of uncontrolled activation of pre-sensitized immune cells by other foreign antigens is high
- SIgAD patients are prone to respiratory tract infections, structural lung disorders (e.g. bronchiectasis) are often observed. Reduced functional lung capacity is a risk factor for poor C0VlD-19 progress.
The paper from Italy also postulates that people with SIgAD are more likely to shed this virus. Why? Less mucosal immunity allows for more viral replication, and thus higher viral loads to shed. This Italian paper notes the following:
“…It has been reported that patients of PAD (Naito et al., 2020), have an increased length of SARS–CoV-2 positivity, before their swab becomes PCR negative, even if this finding may be observed even in the general population of non-immunocompromised subjects. This finding is in fact in agreement with the observation that immunocompromised patients and severe-to-critical patients may remain a source of infection to their environment (Choi et al., 2020). This prolonged viral shedding represents a potential risk for the spreading of the virus in the community, and for virus genetic changes since high rates of mutation might arise, as previously suggested in studies on patients with Primary Immune Deficiencies chronically infected with other viruses, such as chronic OPV infections (Aghamohammadi et al., 2017)…”
Now one of the problems with intramuscular vaccines, like these mRNA vaccines for C-19, is that these vaccines do not provoke much of an IgA antibody immune response in anyone let alone in anyone with SIgAD. Plus whatever small amount of IgA antibodies provoked, don’t appear to be very durable. So people still get infected and can still transmit the virus. However, those infected people who aren’t SIgAD can develop mucosal antibodies. Whereas SIgAD people can’t. So vaccinated SIgAD people most likely will still have more viral replication which, in turn, allows for more random viral mutation that eventually leads to mutations that can evade the RBD spike protein antigens produced by the mRNA and viral vectors vaccines or any other vaccines that solely rely on the 5 or less epitopes of just the spike protein RBD portion of the SARS-CoV-2 virus. These vaccinated SIgAD people, with mutated viruses due to their higher viral loads, will then shed more of this mutated virus.
Anyway, a lot more research is needed to better understand these possible pathways. And that’s what you realize when you actually read the underlying science papers… that is how many open questions there are about this virus, what traits make some people more susceptible, how the vaccines may or may not provoke mutations, what types of antibodies and memory are provoked by natural- hybrid-vaccinated immunity and for how long, what do different viral mutations mean in terms of neutralizing or enhanced immunity, where do the LNPs of mRNA vaccines go and what cells do they transfect, does the S1 cleave and cause inflammation, etc.
Science is about questions…not consensus, absolutes or beliefs.
And there are so many unanswered questions especially about this virus and these genetic vaccine platforms. This is why this is a huge experiment and those who choose to participate are really nothing more than lab rats or chimpanzees.
##